Facilitate nasal breathing in obstructive sleep apnea patients who use oral appliances with these specific designs, accessories, over-the-counter add-ons, and breathing exercise recommendations.
By Alyx Arnett
Persistent mouth breathing presents a challenge in managing obstructive sleep apnea (OSA). This seemingly benign habit—more common in OSA patients1—can exacerbate the severity of the sleep disorder and complicate its treatment.
Often a compensatory response to nasal obstruction and/or a developed habit, mouth breathing can lead to an elongated and narrowed airway, which increases upper airway collapsibility and resistance that further compromises the respiratory stability of OSA patients.2 Mouth breathing has been linked to increased OSA severity, worse oximetric variables, and higher body mass index.3
Nasal breathing, on the other hand, plays an important role in sleep physiology by regulating nasal airway resistance and stimulating ventilation.4 “People ask me how often should you breathe through your mouth, and my answer is as often as you eat through your nose,” says Mark Abramson, DDS, DABOP, DABDSM, DABPM, FAACP, adjunct professor of psychiatry and behavior science at Standford University School of Medicine and president of oral appliance manufacturer Dream Systems. “There’s just a whole list of important physiologic reasons why nasal breathing is critical to health.”
Studies have demonstrated that treating nasal obstruction can significantly reduce mouth breathing during sleep, improve sleep architecture, and improve OSA severity.4 It may also improve the tolerability of CPAP and oral appliances.4
Numerous methods exist to enhance nasal patency—from nasal sprays to surgery. For OSA patients, oral appliances can also be effective.
Built-in Oral Appliance Design Features for Nasal Breathing
Placing an oral appliance between a patient’s teeth may lead to lips parting, which can inadvertently promote mouth breathing. Experts say more compact and less vertical oral appliances foster nasal breathing by limiting how much the mouth opens.
“We know that oral appliances work better under certain types of circumstances: when there’s better nasal breathing—that’s in the literature—when there’s less vertical, and when there’s better lip competency,” says Mark Murphy, DDS, DABDSM, lead clinical faculty for ProSomnus Sleep Technologies and owner of dental sleep practice Funktional Sleep in Rochester Hills, Mich. “If you want somebody to be a really good nasal breather, clean out their nose—whatever they have to do surgically with an ENT—and then good lip competency.”
The ProSomnus EVO Select, with a vertical requirement of only 2.5 millimeters, can help create an environment where nasal breathing can occur, says Murphy. “The lip seal helps to promote nasal patency. Certainly, it doesn’t make a clogged nose open. There’s no magic there, but the less I separate that, the easier it’ll be for you to get lip competency,” he says.

Some oral appliances are designed to pull the mouth closed to promote lip competency. SomnoMed’s SomnoDent Avant uses a 2-millimeter thin strap, anchored anteriorly on the upper and posteriorly on the lower, that couples the appliance to create a fulcrum effect that gently keeps the mouth closed.
“During an apnea event, the mouth opens as the patient typically gasps for air. Other oral devices, if elastics are not used, can allow the mouth to remain open and for the patient to mouth breath,” says Neil Verdal-Austin, CEO and managing director of SomnoMed. “This mouth opening is amplified if the patient is sleeping supine, as the soft palate and tongue fall back on the airway and work against the oral appliance. By closing the mouth and increasing airway patency in the retropalatal/retroglossal areas, the design of the SomnoDent Avant improves OSA, even in supine sleepers.”

Accessories to Encourage Nasal Breathing
Most oral appliances can be customized with accessories like elastics and mouth shields to promote nasal breathing.
Small intraoral hooks for elastics can be fitted to appliances to encourage lip competency. These hooks allow for selectively applying elastic bands that resist the lower jaw’s tendency to open while asleep.
“Almost any type of device can be adapted to encourage mouth closure, resulting in increased nasal breathing by either an attached mechanical feature or using orthodontic elastics,” says Carrie Magnuson, DDS, co-owner of Premier Sleep Associates. “I add hooks or ‘slits’ for orthodontic elastics if the appliance does not have forced mouth closure as part of the inherent design.”
A study using elastics with oral appliances found that oral appliances combined with vertical elastics were significantly more effective at reducing the apnea-hypopnea index (AHI) than oral appliances alone.6 The results were also position-independent, with significant improvements in AHI occurring during both supine and non-supine sleeping positions.
Mouth shields can be used with oral appliances to encourage nasal breathing by reducing airflow through the mouth. Airway Management’s myTAP comes standard with a silicone mouth shield that attaches directly to the device. “The addition of the mouth shield came from the idea of mouth taping but with an easier and more patient-friendly approach,” says Keith Thornton, DDS, inventor of the Thornton Adjustable Positioner (TAP), owner, chief technology officer, and chairman of the board at Airway Management, and owner of dental practice SleepWell Solutions in Dallas.
The combination of an oral appliance with a mouth shield may also have positive implications for brain health. A pilot study showed the therapy could improve cognition in those with dementia.7
Encouraging lip seal prevents dry mouth and excess saliva, common side effects of any oral appliance, which can make the treatment more comfortable and potentially improve adherence.
“Appliances promoting mouth closure and lip seal are ideal. However, the patient’s anatomy needs to be considered, including a short maxillary lip, dental overbite and overjet, posterior clearance, tongue space, retention, and bruxism,” says Magnuson. “With a physical exam and personal history, the appliance is then selected and designed. I also may recommend patients use medical tape to ‘lip tape’ or a mouth shield.”

Opening the Nose from Inside the Mouth
While some products can work independently of oral appliances to help open the nasal airway, a particular oral appliance system, the O2 OASYS Oral/Nasal Airway System, effects nasal patency intra-orally.
Designed by Dream System’s Abramson, the system features two lateral extensions under the upper lip that stretch through the nasolabial fold from inside the mouth to mechanically stretch the nasal valve, which is the area of most restriction, he says. “If you open that, you’re opening everything downstream, and so we’re doing it with these lateral extensions that stretch that area,” says Abramson, who also treats patients at his private practice in Redwood City and Monterey, Calif.
The O2 OASYS Oral/Nasal Airway System was shown to improve nasopharyngeal conditions, such as snoring, upper airway resistance syndrome, and OSA, especially in cases where nasal obstruction was evident.8
It also has demonstrated potential in treating severe OSA cases. In a study, the OASYS Oral/Nasal Airway System resolved almost half (46%) of severe cases with a post-treatment AHI of less than 5, while two-thirds (66%) had an AHI of less than 10. For very severe cases, 43% were resolved with a post-treatment AHI of less than 5, while 64% had an AHI of less than 10.9
“Even if you breathe in through your nose relatively easy, when you go into REM sleep, one of the physiologic characteristics of REM sleep is that sinusoidal tissue swells (increasing nasal resistance),” Abramson says. “It’s been postulated in research that there are two reasons for oral appliance failure. One is obesity, and the other is nasal resistance. So the second most important thing to oral appliance failure is nasal resistance, and we are taking care of that.”
Other methods—paired with oral appliance therapy or used alone—can also help promote nasal breathing.
Mouth taping, a trend in which a person tapes their mouth closed before sleeping to encourage nasal breathing, has gained support from some sleep medicine experts and has even shown efficacy in clinical trials.
One study showed an almost 50% reduction in AHI—from 10.5 events per hour to 5.6 per hour—from oral appliance alone to oral appliance plus mouth taping.9 Another study found that mouth-taping on its own may be able to treat mild sleep apnea patients with mouth breathing, with AHI also being reduced by nearly half.11
“It can be very beneficial. The key is to make modifications based on the patient’s comfort. The tape can be placed differently and changed along the way based on comfort,” says Magnuson. “There are no real risks; they can easily open their mouth or take off the tape.”
Nasal dilators, adhered horizontally across the bridge of the nose, may also give patients relief. “Anything that is going to open your nose will impact the rest of your body and your quality of life greatly,” says Michelle Lovato, founder and inventor of NasalAid, an over-the-counter nasal dilator. “We think NasalAid is the best for those suffering from ongoing rhinitis or collapse of the nasal valve while in the supine position.”
Lovato suggests performing the Cottle test and using the NOSE survey to measure nasal blockage to determine if a patient will benefit from nasal dilators.
Additionally, Magnuson often recommends saline rinses, nasal sprays (medicated and non-medicated), and nasal cones. “Once the patient is comfortable, we can then add (oral appliance) features of locking or encouraging mouth closure, lip taping, or mouth shields,” she says, adding that she also encourages a clean sleep environment and often recommends high-quality air filters.
Magnuson says patients with anatomical concerns might benefit from surgical intervention or recommendations for prescription medications. “If they’ve had a long history of OTC efforts without success, we always encourage an ENT exam,” she says.

Breathing Re-Education
Although oral appliances can promote nasal breathing during sleep, they are not used during waking hours, leaving patients who habitually mouth breathe at risk of improper breathing for around 16 hours a day. “Those 16 hours are contributing to the decline of their health by keeping them in a sympathetic nervous symptom, increasing their heart rate, depression, anxiety, blood PH, etc,” says Michael Flanell, RDH, MBA, president of Advanced Dental Sleep Consultants, certified sleep apnea clinician from the Academy of Clinical Sleep Disorders Disciplines, myofunctional therapist, and certified Buteyko breathing instructor.
For habitual mouth-breathers, relearning how to breathe can be key. Flanell teaches Buteyko techniques, many of which are based on extending the time between inhalation and exhalation, or breath-holding.
One study on breathing re-education suggests patients with sleep apnea should aim to reach a comfortable 25-second breath-hold time after exhaling.12 The researchers say that practicing reduced volume breathing to raise CO2 levels during wakefulness could impact the chemoreceptor response to CO2 during sleep. “Current treatment protocols center on the administration of CO2 after an apnea,” the researchers write. “However, repeated exposure to intermittent hypoxia/hypercapnia on a daily basis over the course of 10 days resulted in a decrease in AHI scores in patients with [sleep apnea].”
Learning how to breathe correctly also complements oral appliance therapy, Flanell says. “If the patient learns to breathe all day nasally, it will make the nighttime breathing more natural and easier for the oral appliance therapy to work more efficiently,” she says. “Depending on the AHI score and why the patient has sleep apnea, in some cases, the oral appliance might not be needed any longer.”
Flanell often encourages her clients to use mouth tape during the day to get them used to breathing through their nose while awake. She also encourages exercises designed to help get their tongue up on the palate, which eventually helps seal off the soft palate to the tongue, expanding the pharynx and keeping it more rigid for breathing, especially at night, she says. “Training the tongue also keeps it from blocking the airways, causing snoring and perhaps other sleep-breathing dysfunctions,” Flanell says.
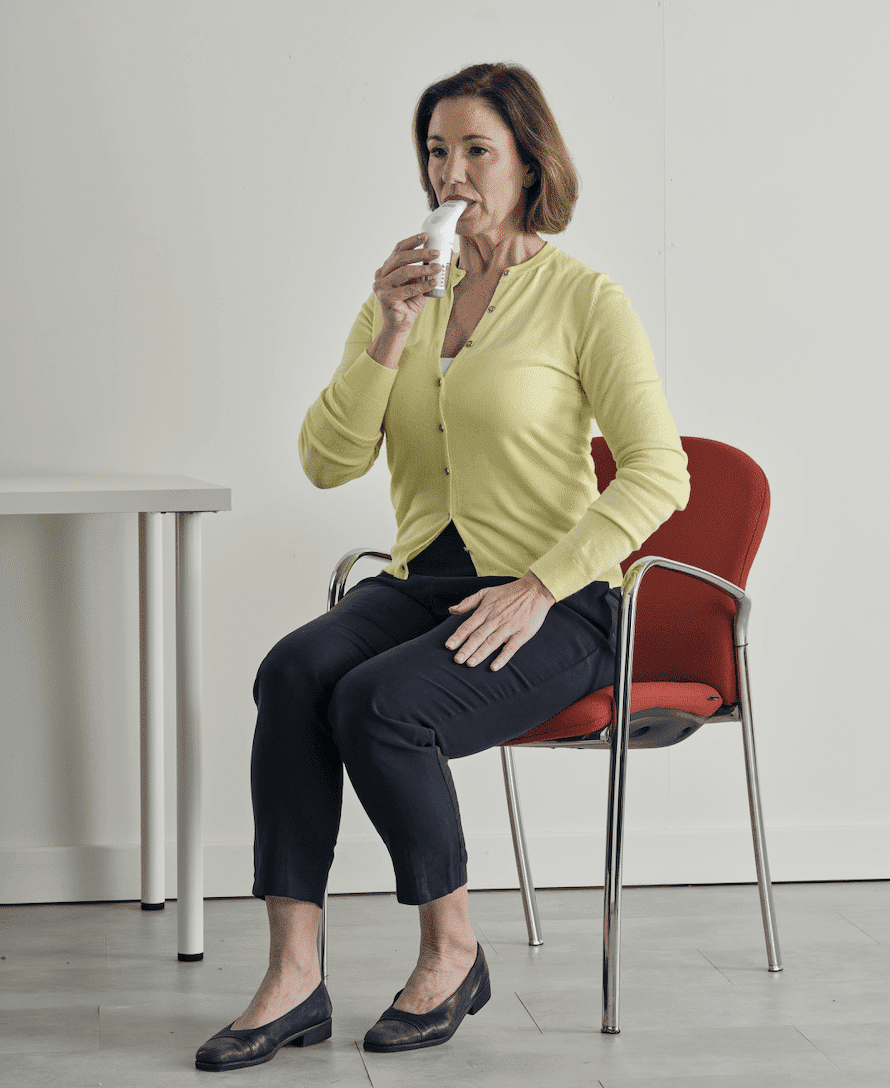
For his patients, Thronton encourages a device called POWERbreathe for inspiratory muscle strength training, which has been shown to strengthen the diaphragm and increase tidal volume.
He also recommends the book “The Breathing Cure” by Patrick McKeown for breathing exercises. “They are simple, non-invasive, patient-friendly, and effective,” he says. “They can improve sleep-disordered breathing and sometimes eliminate the need for an appliance.”
References
- Yi-Fong Su V, Chou KT, Tseng CH, et al. Mouth opening/breathing is common in sleep apnea and linked to more nocturnal water loss. Biomed J. 2023 Jun;46(3):100536.
- Suzuki M, Tanuma T. The effect of nasal and oral breathing on airway collapsibility in patients with obstructive sleep apnea: Computational fluid dynamics analyses. PLoS One. 2020 Apr 13;15(4):e0231262.
- Hsu YB, Lan MY, Huang YC, et al. Association between breathing route, oxygen desaturation, and upper airway morphology. Laryngoscope. 2021 Feb;131(2):E659-E64.
- Cai Y, Goldberg AN, Chang JL. The nose and nasal breathing in sleep apnea. Otolaryngol Clin North Am. 2020 June;53(3):385-95.
- McLean HA, Urton AM, Driver HS, et al. Effect of treating severe nasal obstruction on the severity of obstructive sleep apnoea. Eur Respir J. 2005 Mar;25(3):521-27.
- Milano F, Mutinelli S, Sutherland K, et al. Influence of vertical mouth opening on oral appliance treatment outcome in positional obstructive sleep apnea. J Dent Sleep Med. 2018;5(1):17-23.
- Schramm P, Das N, Schneiderman E, et al. Snoring remediation with oral appliance therapy potentially reverses cognitive impairment: an intervention controlled pilot study. Geriatrics. 2021 Nov 1;6(4):107.
- Singh GD, Abramson M. Effect of an intra-oral nasal dilation appliance on 3-D nasal airway morphology in adults. Sleep Breath. 2008 Mar;12(1):69-75.
- Shrivastava D, Bixby JK, Livornese DS, et al. Efficacy of oral appliance therapy in the treatment of severe OSA in CPAP-resistant cases. Sleep Vigilance. 2018 July 26;2: 119–25.
- Labarca G, Sands SA, Cohn V, et al. Mouth closing to improve the efficacy of mandibular advancement devices in sleep apnea. Ann Am Thorac Soc. 2022;19(7):1185-92.
- Lee YC, Lu CT, Cheng WN, Li HY. The impact of mouth-taping in mouth-breathers with mild obstructive sleep apnea: a preliminary study. Healthcare. 2022 Sep;10(9):1755.
- McKeown P, O’Connor-Reina C, Plaza G. Breathing re-education and phenotypes of sleep apnea: a review. J Clin Med. 2021;10(3):471.
Photo caption: Profile photos of a patient wearing a previous oral appliance (left) and the ProSomnus EVO Select (right) show how the smaller design of the ProSomnus EVO Select helps promote lip competency.
Photo credit: ProSomnus